Thrombosis is the major cause of morbidity and mortality in Chuvash erythrocytosis (CE), caused by a hypomorphic R200W mutation of the Von Hippel-Lindau (VHL) gene, a negative regulator of hypoxia inducible factors (HIFs). This mutation augments HIF activity even in normoxia. High hematocrit associated with hyperviscosity has been considered a risk factor for thrombosis suggesting that maintaining normal hematocrit may prevent thrombosis. However, our prospective controlled study reported that phlebotomies, but not the high hematocrit, are associated with increased risk of thrombosis (PMID 289208) by a mechanism that remains to be elucidated.
Phlebotomies lead to iron deficiency. We explored the potential role of iron deficiency as a cause of thrombosis. Iron deficiency induces HIF activity by inhibiting prolyl hydroxylase domain 2 (PHD2), an inhibitor of HIFs that requires iron as a co-factor (PMID 18066546). The expression of certain prothrombotic genes regulated by HIFs is modestly increased in CE mononuclear cells (PMID 23993337). We hypothesized that further augmentation of already high HIF activity by iron deficiency might further increase expression of prothrombotic genes leading to increased risk of thrombosis in phlebotomized subjects.
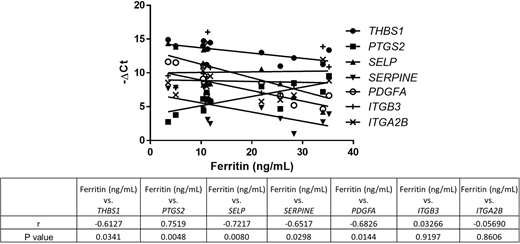
We reported that, in polycythemia vera (PV) and essential thrombocythemia (ET), the pattern of increase in prothrombotic and inflammatory gene expression differs between granulocytes and platelets (PMID: 32203583), suggesting cell-specific contributions to thrombosis in these disorders. We analyzed the whole transcriptome of the platelets of 10 CE patients, 6 with iron deficiency (ferritin <20 ng/ml) and 4 with normal ferritin: 2,412 genes were upregulated and 670 were downregulated (p <0.05 and Log2 fold change >1). Dysregulated genes as analyzed by Ingenuity Pathway Analysis (Qiagen) were associated with platelet binding, hemostasis and thrombus signaling and decreased bleeding time. To explore our hypothesis further, we quantitated the mRNA of these HIF-regulated prothrombotic genes: THBS1 (thrombospondin 1), SERPINE1 (plasminogen activator inhibitor-1 [PAI-1]), ITGA2B (integrin alpha-IIb), PTGS2 (prostaglandin-endoperoxide synthase 2), SELP (P-selectin), PDGFA (platelet derived growth factor subunit A), and ITGB3 (integrin beta-3). We analyzed granulocytes from 16 CE subjects (8 iron deficient) and platelets from 12 CE subjects (7 iron deficient). In platelets, THBS1, SELP, SERPINE1, and PDGFA mRNA levels were higher in iron deficient CE subjects than those with normal ferritin (p=0.015-0.088). In all CE subjects, the mRNA levels of these four genes correlated inversely with ferritin (figure 1). PTGS2 (known to be down regulated in thrombosis) was down regulated in iron deficient CE patients and correlated positively with ferritin. ITGB3 and ITGA2B mRNA levels were not different between the two groups. In granulocytes, SELP mRNA was augmented in CE patients with iron deficiency and both SELP and ITGB3 mRNA levels correlated inversely with ferritin. We did not find a difference in expression of KLF2, a regulator of thrombotic genes, in iron deficient versus iron sufficient CE patients; see this meeting Song J et al.
We then tested our hypothesis of augmentation of thrombosis risk by iron deficiency in granulocytes from 50 PV and ET patients (9 with iron deficiency) and platelets from 41 patients (5 with iron deficiency). In granulocytes, THBS1, SELP, and IRAK1 (Interleukin 1 Receptor Associated Kinase 1) mRNA levels were higher in patients with iron deficiency, and IRAK1, THBS1, and SERPINE1 mRNA levels correlated inversely with ferritin. In platelets, THBS1, and SERPINE1 mRNA were higher in patients with iron deficiency and SELP, THBS1, and SERPINE1 mRNA levels correlated inversely with ferritin. JAK2V617F allele burden also correlated inversely with ferritin.
Our study demonstrates that iron deficiency is associated with increased expression of HIF-regulated prothrombotic genes in CE platelets and granulocytes in a pattern that differs between these two cell types. We also report increased expression of prothrombotic genes in PV and ET patients with iron deficiency. These results underline the potential danger of phlebotomies in attempts to control high hematocrit. We caution against indiscriminate use of therapeutic phlebotomy for treatment of patients with PV and other erythrocytoses.
VG &JTP contributed equally
Gordeuk:Ironwood: Research Funding; Novartis: Consultancy; CSL Behring: Consultancy, Research Funding; Global Blood Therapeutics: Consultancy, Research Funding; Imara: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.